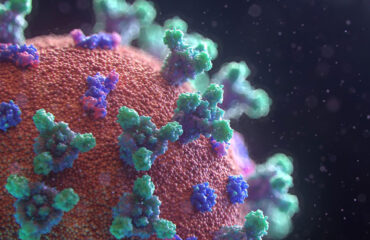
On 11 March 2020, the outbreak of coronavirus disease (COVID-19) has been declared a global pandemic by the World Health Organization as the virus has spread to many countries. It’s the first time the WHO has called an outbreak a pandemic since the H1N1 “swine flu” in 2009.
What is confirmed is that the virus is transmitted through direct contact with respiratory droplets of an infected person (generated through coughing and sneezing). Individuals can also be infected from and touching surfaces contaminated with the virus and touching their face (e.g., eyes, nose, mouth). Besides, the COVID-19 virus may survive on surfaces for several hours, yet disinfectants can kill it.
On 9 March, the European Food Safety Agency (EFSA) stated on their website that there is currently no evidence that food is a likely source or route of transmission of the novel coronavirus, and that they are closely monitoring the situation as any new information about the outbreak comes to light. EFSA’s opinion is based on the fact that previous outbreaks of related coronaviruses, such as severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV), show that transmission through food consumption did not occur. BfR, the federal institute of risk assessment in Germany concurred with the findings, stating that there are currently no cases that have shown any evidence of humans being infected with the new type of coronavirus by another method, such as via the consumption of contaminated food or via imported toys. Transmission via surfaces which have recently been contaminated with viruses is, nonetheless, possible through smear infections. This is only likely to occur during a short period after contamination, due to the relatively low stability of coronaviruses in the environment.
WHO Director General
A recent review analyzed 22 studies and revealed that human coronaviruses such as Severe Acute Respiratory Syndrome (SARS) coronavirus, Middle East Respiratory Syndrome (MERS) coronavirus or endemic human coronaviruses (HCoV) can persist on inanimate surfaces like metal, glass or plastic for up to 9 days, but can be efficiently inactivated by surface disinfection procedures with 62–71% ethanol, 0.5% hydrogen peroxide or 0.1% sodium hypochlorite within 1 minute. Other biocidal agents such as 0.05–0.2% benzalkonium chloride or 0.02% chlorhexidine digluconate are less effective
This is what we know “so far”. As the WHO Director-General stated “This virus is not SARS, it’s not MERS, and it’s not influenza. It is a unique virus with unique characteristics”, and scientists are working around the clock to address critical gaps in knowledge.
In a recent study (US government work) conducted by the National Institutes of Health, Princeton University and the University of California, Los Angeles, with funding from the U.S. government and the National Science Foundation, Covid-19 was detected up to three hours later in the air, up to four hours on copper, up to 24 hours on cardboard and up to two to three days on plastic and stainless steel.
Revise and update the health policy
Having said that, while there is a lot of uncertainty in the situation, it is advisable that food processors evaluate the current practices inside their organization and manage staff who may be carriers or infected with the Coronavirus. Reviewing and updating the existing disease control/health policy while considering recent recommendations and requirements of the local authorities is paramount. Did you address in your your policies address any food to which an ill employee may have had exposure, including whether the policies address whether there are conditions present that would support a company decision to place food on hold pending advice from the public health authorities.
Here are the CDC recommended strategies for employers to use which may help may help prevent workplace exposures to acute respiratory illnesses, including COVID-19. Many of the steps described in the CDC link are useful and apply to every food facility, yet as a food facility outside the US, you will refer to the guidance, updates and travelers’ health notices of local authorities to determine whether there are any local requirements to contact public health authorities in the event an employee in the workplace has been diagnosed with COVID-19 and to establish procedures for handling other employees who may have come in contact with the diagnosed employee.
Top management should encourage employees with symptoms to stay home and get prepared for the sudden absenteeism and shortage of staff.
Besides the disease control plan, precautionary hygiene measures are of significant importance.
The World Health Organisation (WHO) has issued recommendations including advice on following good hygiene practices during food handling and preparation, such as washing hands, cooking meat thoroughly and avoiding potential cross-contamination between cooked and uncooked foods. Similarly, many local authorities such as in Belgium also emphasized those practices.
As simple as this seems to be, translating messages into practices is not easy and often undermined with barriers that need to be understood. In practice, it requires instilling a hygiene culture to ensure the highest levels of hygiene measures, particularly when food processors may face the situation of operating with staff shortages and absenteeism. A hygiene culture in a way it does not require the staff to think much about it! it is a culture shared at all levels of the organization from top management to production staff. Have you included in your contingency plan re-evaluating your hygiene standards?
The topic of today is focused on hand hygiene, which must not be overlooked in your Covid-19 training tool box. What have you done to highlight this issue in your organization? It would be great if you share your experience with others in the comment box.
I am sharing some of the key messages you may like to consider to reinforce the hand washing practices:
Hygiene Culture
1- Assign competent staff to stay aware of recent news and updates on the COVID-19 outbreak, how it is transmitted and how to prevent transmission. Information are available on the CDC, ECDC, WHO websites, and local health authorities. Use facts from a credible source for sound decision making.
2- Develop a culture of safety around hand hygiene shared all levels of the organization from top management to production staff.
Handwashing with soap and water is still the best way to prevent transmission of the virus, according to the Centers for Disease Control and Prevention.
Get involved as management in monitoring the compliance levels and identify risk areas in staff behaviors. You may come up with measurement tools or refer to other tools such as the “notational observation” checklists. This may not be easy though. I recommend you to check the WHO Hand
hygiene self-assessment framework and compliance observation tools.
Yes! This framework is a tool to obtain a situation analysis of hand hygiene promotion and practices within an individual health-care facility, according to a set of indicators. But I see this an effective tool that can be adapted to use in food facilities too. It also acts as a diagnostic tool, identifying key issues requiring attention and improvement. Repeated use of the Framework will allow documentation of progress with time.
Adapting this tool to your organization might be of great value to leverage the hand hygiene practices and work on ensuring a hygiene culture that prevails.
3- Review the existing hygiene policy, update it, and reinforce the rules of hygienic practices and requirements. Circulate the rules so that all employees (top and middle management staff and operators) read it, sign it again, and discuss it all over again. Assess whether your policy considers how to manage staff who may have come in contact with an employee diagnosed with a communicable disease.
Those rules are essential to creating a safe and hygienic environment to ensure food safety.
Consider reviewing the risks in the food dining area, if applicable. Is it a self-service dining area? Is the food covered or uncovered? Is there a risk of hands touching cold items when picked from the display? Same with the fruits and bread baskets.
4- Training training training. The WHO, CDC, and local authorities websites have generous information that can be of use in your communications with the food workers and management staff. Program REGULAR training on the importance of hand hygiene, based on the five simple steps , and the correct procedures for hand-rubbing and handwashing, to all food workers.
Use infographics and videos such as those available on the CDC website to convey powerful messages on handwashing, prompting and reminding food workers about the importance of hand hygiene and about the appropriate indications and procedures for performing it.
5- Establish a daily meeting with all the staff e.g. management and operators for conveying key and new messages. Listen to their concerns and challenges to identify barriers and draft a new strategy to promote a hygiene culture.
The perception of risks differ greatly among people working in the same organization. My experience showed that even quality assurance staff may take a particular behavior for granted when it should be prudently exercised, such as visiting the toilet with the shoe covers and re-entering food premises without replacing them. Underestimating the risks is a result of inadequate training or “framed” classical training. Talk science with the staff using data and easy to understand materials.
The posters and signs, and key messages in transient areas and inside the plant are not enough. Discuss them, alternate messages across the areas, use news headlines, share with food workers recent scientific opinions on Covid-19 using a simple language and hygiene risks to avoid. See sample posters here for use.
6- Ensure that team leaders are well trained and knowledgeable to communicate the important aspects of employee hygiene and food safety to production team members and explain how unhygienic or failure to exercise proper hygiene reflect on your organization, customers and products. They should be capable of picking up examples on risks and how this may reflect on hand hygiene and food safety.
References:
- https://www.cdc.gov/coronavirus/2019-ncov/index.html
- https://www.who.int/health-topics/coronavirus
- www.FMI.org/Coronavirus
- https://www.cdc.gov/handwashing/index.html
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public